Introduction
Cross-sectional imaging, especially contrast-enhanced CT (CECT) and MRI, is crucial in evaluating neck masses. Understanding the deep neck spaces is the first step in narrowing the differential diagnosis. Among these, the parapharyngeal space (PPS) is a central “hub,” and lesions here often displace or invade adjacent compartments.
CT Neck Spaces: Anatomical Overview
Neck spaces are defined by the deep cervical fascia. On CT (axial sections), recognizing fat planes and fascial boundaries helps localize disease.
Major Neck Spaces
- Pharyngeal Mucosal Space
- Contains: nasopharynx, oropharynx, hypopharynx mucosa & lymphoid tissue.
- Pathology: squamous cell carcinoma, lymphoma.
- Parapharyngeal Space (PPS)
- “Inverted pyramid” space between pharyngeal mucosal space (medial) and masticator/parotid spaces (lateral).
- Fat-filled space, key landmark in mass effect.
- Masticator Space
- Muscles of mastication (masseter, pterygoids), ramus of mandible, CN V3.
- Pathology: sarcomas, odontogenic infections.
- Parotid Space
- Parotid gland, facial nerve branches.
- Pathology: pleomorphic adenoma, Warthin tumor, parotitis.
- Carotid Space (Vascular Space)
- Internal carotid artery, internal jugular vein, CN IX–XII, sympathetic chain.
- Pathology: schwannomas, paragangliomas, carotid body tumors.
- Retropharyngeal Space
- Between buccopharyngeal & alar fascia.
- Extends skull base → mediastinum.
- Pathology: abscess, metastasis.
- Danger Space
- Between alar & prevertebral fascia.
- Infection can track to mediastinum.
- Prevertebral Space
- Prevertebral muscles, vertebral bodies.
- Pathology: chordoma, osteomyelitis, abscess.
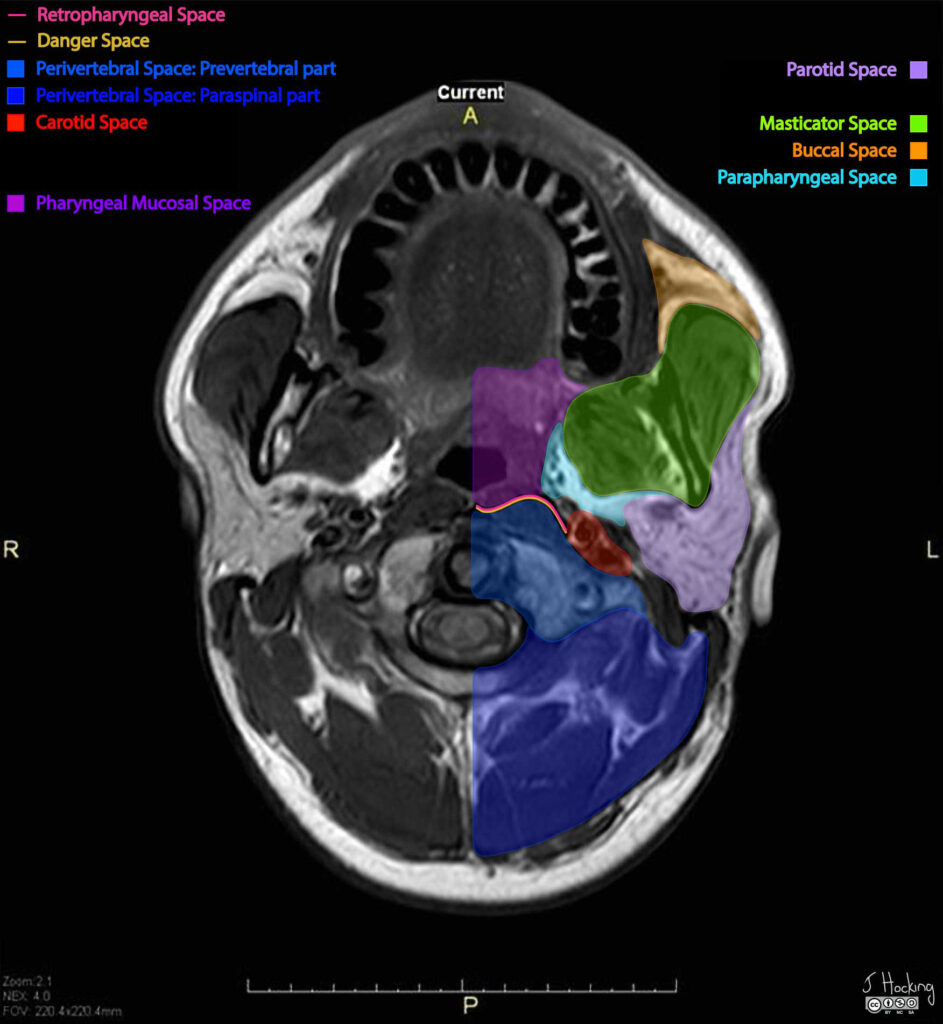
Case courtesy of Jeffrey Hocking, Radiopaedia.org. From the case rID: 43811
Parapharyngeal Space (PPS) in Detail
- Shape: Inverted pyramid
- Base = skull base
- Apex = greater cornu of hyoid
- Compartments:
- Prestyloid → fat, minor salivary glands, branches of CN V3, ascending pharyngeal artery.
- Poststyloid → carotid sheath contents, CN IX–XII, sympathetic chain.
Imaging Features of Parapharyngeal Lesions
1. Displacement of Fat as a Diagnostic Sign
- PPS fat plane displacement helps localize the origin of lesions:
- Medial displacement → lesion from parotid space.
- Anterior displacement → lesion from carotid space.
- Lateral displacement → lesion from pharyngeal mucosal space.
- Posterior displacement → lesion from masticator space.
2. Common PPS Lesions
Prestyloid Compartment
- Pleomorphic adenoma (most common PPS tumor; often from deep lobe of parotid).
- Lipoma, minor salivary gland tumors.
Poststyloid Compartment
- Neurogenic tumors → schwannomas (vagus, sympathetic chain).
- Paragangliomas → carotid body tumor, glomus vagale, glomus jugulare (if skull base extension).
- Metastatic nodes / Lymphoma.
Key CT Findings
- CT with IV contrast shows:
- Lesion density, enhancement, calcification.
- Bony erosion (important for skull base/parotid extension).
- Fat displacement sign for compartment localization.
📝 Teaching Points
- Neck space anatomy on CT is based on fascial planes and fat compartments.
- PPS lesions are classified into prestyloid vs poststyloid, which narrows the differential.
- Fat displacement pattern is the single most useful imaging sign in PPS mass localization.
✅ Conclusion
Understanding CT neck space anatomy and parapharyngeal lesion localization is crucial for accurate diagnosis and surgical planning. Radiologists must carefully analyze fat displacement, enhancement patterns, and compartment involvement to arrive at the right differential.
