Introduction
The neck contains multiple potential spaces formed by the layers of deep cervical fascia. These fascial spaces act as natural boundaries for the spread of infection, tumors, or fluid collections. Understanding their anatomy on CT and MRI is crucial for accurate localization and differential diagnosis of neck pathology.
FASCIAL LAYERS OF THE NECK
1. Superficial cervical fascia
- Lies just beneath the skin.
- Contains platysma muscle, superficial veins, lymphatics, and cutaneous nerves.
- Not typically seen on CT/MRI unless thickened by edema or inflammation.
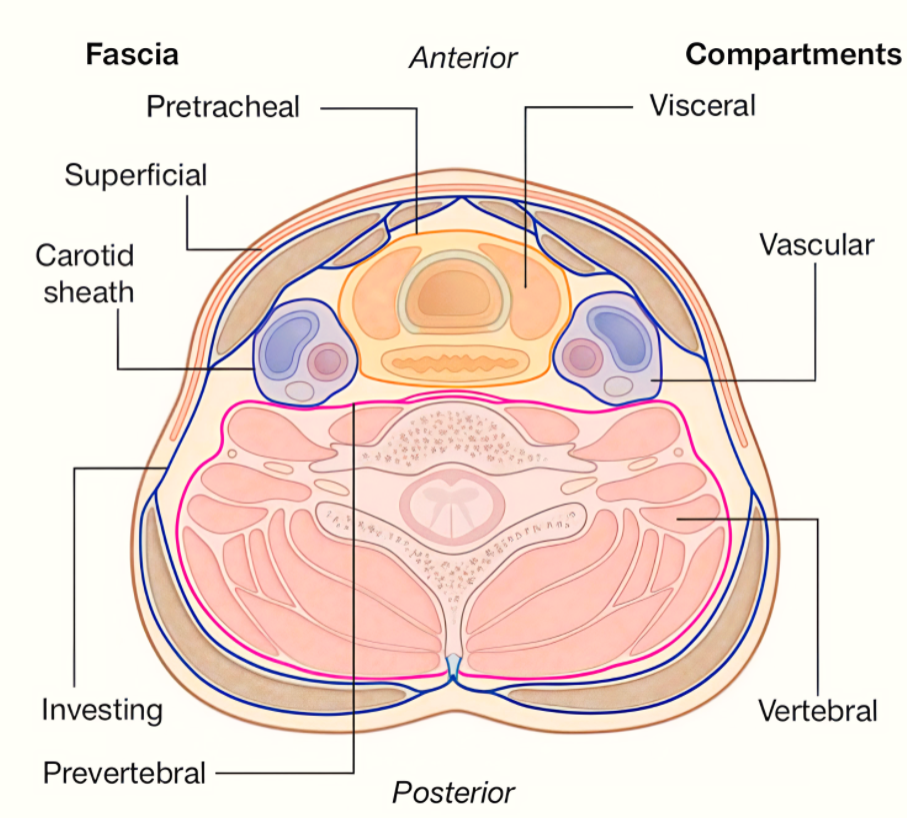
2. Deep cervical fascia – Divided into three layers:
- Investing layer: Encircles the entire neck, enclosing sternocleidomastoid (SCM) and trapezius muscles.
- Pretracheal layer: Surrounds thyroid gland, trachea, and esophagus (visceral compartment).
- Prevertebral layer: Encloses vertebral column and deep muscles of the neck.
- Carotid sheath: A condensation of all three layers enclosing common/internal carotid artery, internal jugular vein, and vagus nerve.
MAJOR CERVICAL FASCIAL SPACES & CT/MRI FEATURES
1. Masticator Space
- Boundaries: Investing layer of deep cervical fascia.
- Contents: Masseter, medial & lateral pterygoid muscles, ramus of mandible, CN V3 branches.
- Best seen on: Axial CT (bone & muscle anatomy), MRI for muscle signal.
- Pathologies: Odontogenic infections, sarcomas, perineural tumor spread along mandibular nerve.
2. Parapharyngeal Space (PPS)
- Shape: Inverted pyramid (base at skull base, apex at hyoid).
- Divisions: Pre-styloid and post-styloid compartments.
- Contents: Fat (pre-styloid), carotid sheath structures (post-styloid).
- CT/MRI Clues: Fat attenuation (CT), high T1 signal (MRI). Displacement of PPS fat helps localize masses:
- Medial displacement: Masticator space lesion.
- Anterior displacement: Carotid space lesion.
3. Retropharyngeal Space
- Location: Between buccopharyngeal fascia and alar fascia. Extends from skull base to T3.
- Contents: Fat, lymph nodes.
- Clinical significance: Route for spread of infections to mediastinum.
- CT/MRI appearance: Fat density or high T1 signal; pathological thickening or fluid collection.
4. Danger Space
- Location: Between alar fascia and prevertebral fascia.
- Extent: Skull base to diaphragm.
- Importance: Potential pathway for rapid spread of infection to mediastinum.
- Imaging: Difficult to distinguish from retropharyngeal space; diagnosed when infection extends below T3.
5. Carotid Space
- Contents: Carotid artery, internal jugular vein, vagus nerve, sympathetic chain.
- Pathologies: Paragangliomas (carotid body tumors), nerve sheath tumors, vascular lesions.
- CT/MRI: On MRI, vessels show flow voids; tumors may splay carotid bifurcation (“lyre sign”).
6. Prevertebral Space
- Location: Between prevertebral fascia and vertebral bodies.
- Contents: Prevertebral muscles, vertebrae.
- Pathologies: Trauma, discitis, vertebral osteomyelitis, tumor extension.
- MRI: Excellent for soft tissue and marrow involvement.
7. Sublingual & Submandibular Spaces
- Sublingual space: Between mylohyoid muscle and oral mucosa; contains sublingual gland.
- Submandibular space: Between mylohyoid and investing fascia; contains submandibular gland, lymph nodes.
- Pathologies: Sialadenitis, abscess, ranula.
ROLE OF CT
- Advantages:
- Excellent spatial resolution.
- Visualizes bony structures and calcifications.
- Rapid acquisition for emergency cases.
- Limitations:
- Limited soft tissue contrast compared to MRI.
- Radiation exposure.
ROLE OF MRI
- Advantages:
- Superior soft tissue contrast – ideal for tumor extent and nerve involvement.
- Multiplanar imaging without repositioning.
- Fat suppression sequences improve lesion detection.
- Sequences used:
- T1-weighted: Anatomy, fat planes.
- T2-weighted: Edema, cystic lesions.
- STIR/Fat sat: Better visualization of inflammation.
- Post-contrast T1: Enhancing masses, vascular lesions.
SUMMARY TABLE
| Space | Key Structures | CT Utility | MRI Utility |
|---|---|---|---|
| Masticator | Muscles, CN V3 | Bone + muscle anatomy | Perineural spread |
| Parapharyngeal | Fat, carotid sheath | Fat displacement | Compartment localization |
| Retropharyngeal | Fat, LN | Abscess detection | Soft tissue edema |
| Danger space | None (fat) | Extension below T3 | Mediastinal tracking |
| Carotid | ICA, IJV, CN X | Vessel anatomy | Flow voids, tumor characterization |
| Prevertebral | Muscles, vertebrae | Fractures, alignment | Infection, tumor |
| Sublingual/Submandibular | Salivary glands | Sialolithiasis | Gland inflammation |
KEY EXAM POINTS
- Recognizing fat plane displacement is crucial to localize lesions.
- CT excels at bone and calcifications; MRI excels at soft tissue and perineural spread.
- Fascial space knowledge guides surgical planning and predicts spread of infection or tumor.
